Photo courtesy of Lymphedivas
After her mastectomy, Peggy, age 62, developed significant lymphedema that she attributes to doing the plank pose as part of her physical therapy regimen. Kathy, age 57, developed lymphedema in her legs a decade after having almost 20 nodes removed from her inguinal area, and she has no idea what triggered it. Chris, age 47, a lifelong athlete, does handstand pushups with no symptoms of swelling after having had thirteen lymph nodes removed during her breast cancer surgery two years earlier.
Although many people with lymphedema enjoy active lives, lymphedema can be both physically and psychologically distressing. You may have experienced the effects of lymphedema personally, or, you may have seen a woman wearing a compression sleeve (which now, thanks for companies like Lymphedivas, come in fashionable patterns). Garments like these are worn to help control lymphedema—which is a potential side effect of cancer treatments, such as surgery or radiation, which can injure the lymphatic system. Cancer treatments such as lymph node removal and radiation are the leading causes of “secondary” lymphedema, whereas primary lymphedema results from a congenital defect and is much less common.
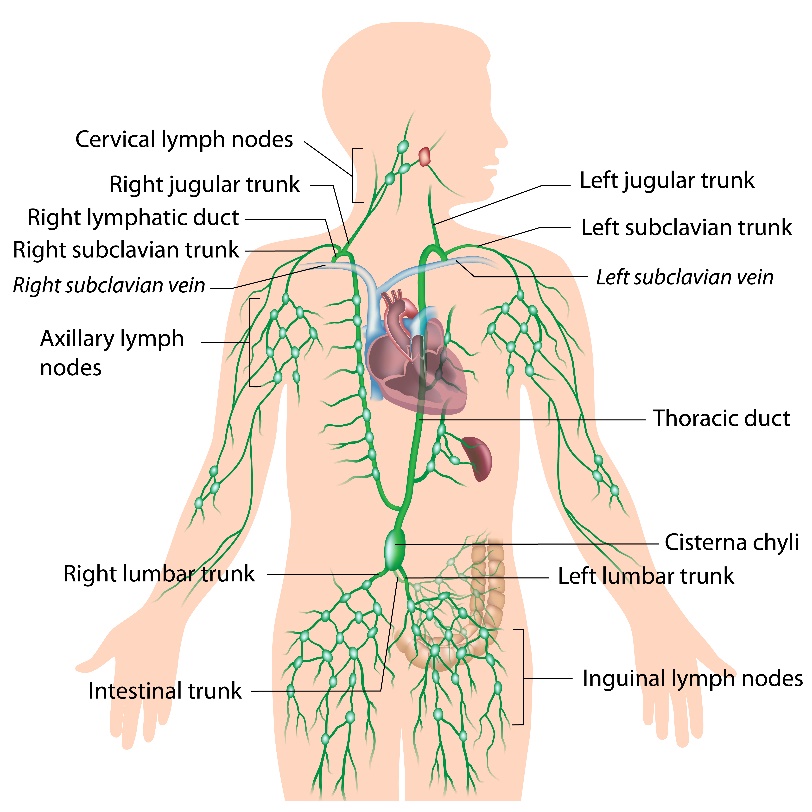
Understanding the Lymphatic System
The lymphatic system is one of the unsung heroes of the body. Part of the immune system, it acts as part of the body’s cleaning and protection team, transporting waste from cells and combating infection. The lymphatic system typically contains 600-700 lymph nodes throughout the body, with larger clusters found in the cervical (neck), axilla (armpits), mediastinal (chest) and inguinal (groin) areas. The lymphatic system does not have its own central pump, as the circulatory system does, so that lymph movement occurs due to peristalsis (contraction and relaxation of smooth muscle) and valves, which prevent back-flow.
Image of the Lymphatic System
How Lymphedema Develops
According to the National Lymphedema Network (NLN), a leading advocacy organization for the condition, lymphedema results from “an abnormality of lymphatic system leading to excessive buildup of tissue fluid that forms lymph, known as interstitial fluid.” Instead of the lymphatic system moving this protein-rich fluid to the thoracic duct, the largest lymphatic vessel in the center of the chest, for recirculation, this fluid becomes stagnant and remains in the cell tissue, causing swelling and increased risk of infection. Lymphedema can occur in the quadrant of the body where the lymph nodes have been damaged. For example, it can occur in the arms and chest after breast cancer treatment, in the legs after pelvic area cancer treatments, and in the chin and face after head and neck cancer treatments.
Lymphedema Risk
There is no definitive way to predict who will develop lymphedema; some persons with few lymph nodes affected or removed develop the disorder while those with many more lymph nodes removed or affected do not. One factor is that every individual’s distribution of lymph nodes is unique; studies show that in the axilla (under the arm) there may be as few as eight lymph nodes or as many as 53, with an average of about 25-30 lymph nodes on each side. The NLN, which creates position papers based on hundreds of lymphedema-related studies, established that the overall risk of lymphedema due to all cancers is 15.5%. However, that percentage can vary greatly by the type of cancer and the treatment.
The International Society of Lymphology states that among premenopausal breast cancer survivors, 54% reported swelling within three years after surgery. Research shows that the risk of lymphedema increases with the removal of more lymph nodes. A 2010 study published in Cancer Epidemiology Biomarkers & Prevention showed that up to 89% of those studied experienced lymphedema after an axillary lymph node dissection (ALND), which is a removal of 6 or more lymph nodes. In contrast, other studies found lymphedema occurred in only 4-11% of people who received the less invasive sentinel node biopsy (SNB), in which five or fewer lymph nodes are removed.
Radiation treatments can create additional lymph system damage and further increase the lymphedema risk. Multiples surgeries, procedures, treatments, infections, injuries and being overweight also increase risk.
Lymphedema Risk Reduction versus Prevention
Experts use the term “risk reduction” rather than “prevention” because no guarantee of prevention exists. Individuals with very few risk factors can experience lymphedema, while others with many more risk factors do not.
However, because there is some correlation between risk factors and the probability of experiencing lymphedema, the NLN risk reduction position paper, last revised in May, 2012, states:
Because of individual variations in anatomy and because lymphedema may be caused by many different factors, each person with lymphedema or at risk for lymphedema needs to have their risk-reduction practices individualized. What works for one person may not work for another… Lymphedema is a progressive condition without a cure; caution should be exercised to reduce the risk of developing or exacerbating lymphedema [bold added].
Once the lymph nodes have been removed or injured, the risk of lymphedema is a lifelong risk and those at risk will need to take appropriate precautions.
Changing What May Be the Biggest Risk Factor for Lymphedema
Linda Roherty, PT, CLT-LANA, a frequent speaker and an international authority on lymphedema, calls the biggest risk for lymphedema “a knowledge deficit.” Linda and other lymphedema experts emphasize the critical importance of education on the topic for all individuals who may be at risk — which includes a large proportion of those who have had cancer treatment. Understanding what precautions to take and how to manage your risk factors are keys to risk reduction.
Linda Roherty strongly advises individuals at risk of lymphedema to “know your limb.” That means getting intimately familiar with what is feels like and what affects it — to pay attention to the size of the limb, to have it measured before treatment if possible, watch closely for anything that makes it swell, feel numb, makes rings get tight or causes the skin to feel taut or uncomfortable.
Once someone has lymphedema, it never “goes away” but it can be managed and possibly reversed to earlier stages with appropriate treatment — so it is critically importance to understand the risk factors and get educated on the early signs and symptoms of the condition.
Getting the appropriate treatment by a qualified health professional who specializes in lymphedema at the earliest possible stage is key to minimizing the potential effects of the condition. Wellness professionals who deal with people with or at risk for lymphedema should be educated on the basics of the condition and take the appropriate precautions as indicated.
Lymphedema Management Resources: For Practitioners
Lymphedema Management: The Comprehensive Guide for Practitioners
Lymphedema: Complete Medical and Surgical Management
Lymphedema Management Resources: For Patients
Restorative Yoga For Breast Cancer Recovery: Gentle Flowing Yoga For Breast Health, Breast Cancer
Related Fatigue & Lymphedema Management
100 Questions & Answers About Lymphedema