Why do some people heal from dire diagnoses, despite all odds?
Ten years ago, that was a question that Kelly Turner wanted an answer to, and she set out to answer it. By now, you have likely heard about the results of her research and the phenomena known as Radical Remission that is sweeping the country and world.
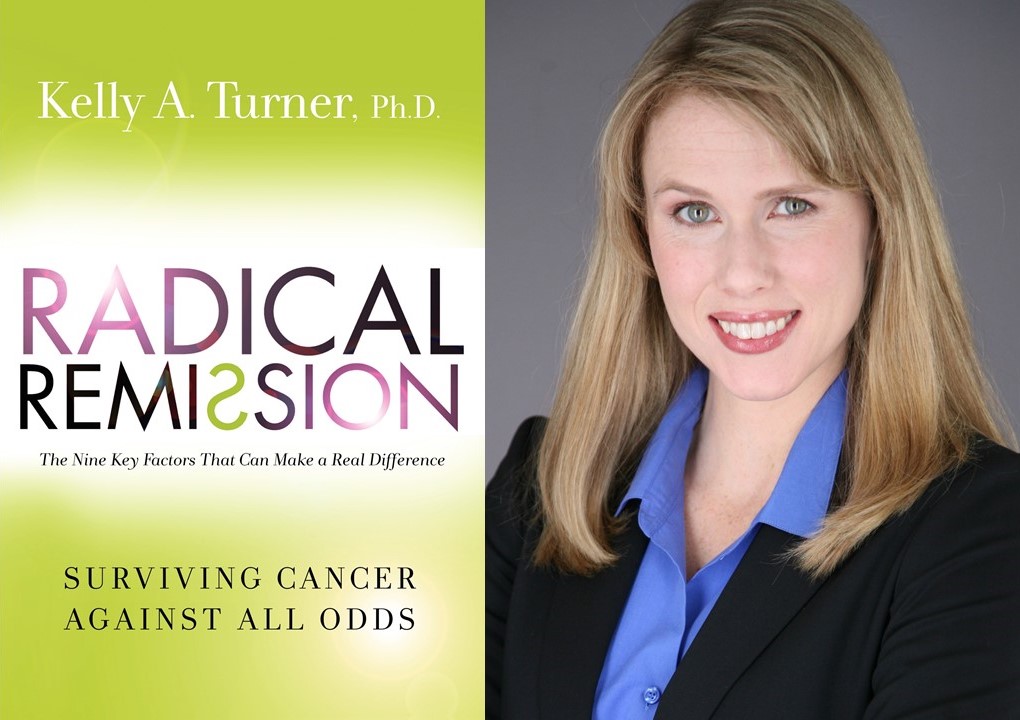
Kelly Turner, PhD, author of the New York Times bestseller, Radical Remission: Surviving Cancer Against All Odds, is a researcher, psychotherapist and writer who specializes in integrative oncology. For a decade, Dr. Turner has studied “radical remission”— when cancer goes away despite medical expectations — cases that could be described as a medical “anomaly,” whether or not that person received conventional medical treatments.
 Dr. Kelly A. Turner, Ph.D. is a researcher, lecturer, and counselor in the field of Integrative Oncology whose specialized research focus is the radical remission of cancer. Dr. Turner holds a B.A. from Harvard University and a Ph.D. from the University of California, Berkeley. She lives in New York City.
Dr. Kelly A. Turner, Ph.D. is a researcher, lecturer, and counselor in the field of Integrative Oncology whose specialized research focus is the radical remission of cancer. Dr. Turner holds a B.A. from Harvard University and a Ph.D. from the University of California, Berkeley. She lives in New York City.
More at www.kelly-turner.com and www.RadicalRemission.com.
Working first as a psychotherapist with oncology patients, Dr. Turner vowed to help her patients find out what factors could potentially turn around a life-threatening cancer diagnosis. Returning to graduate school for her doctorate, Dr. Turner traveled the globe for a year, collecting data for her dissertation. Besides talking to Radical Remission survivors, Dr. Turner also interviewed fifty non-Western alternative healers from the jungles, mountains and cities of countries including the United States, China, England, Brazil, India and Zimbabwe.
Dr. Turner’s book summarizes the results of her research: interviews with one hundred cancer survivors and analysis of now over one thousand cases of people who experienced a radical remission. The survivors Dr. Turner talked to were those who, because of the type and/or stage of their cancer, were considered by conventional medicine unlikely to heal from it — yet, despite all odds, they had.
In her research, Dr. Turner found that 75 healing factors appeared in these cases, but nine were common among all of the cases she studied. She calls them, “The Nine Key Factors That Can Make a Real Difference.”
 According to Dr. Turner, almost all the Radical Remission survivors that she interviewed mentioned doing these same nine things in order to heal their cancer.
According to Dr. Turner, almost all the Radical Remission survivors that she interviewed mentioned doing these same nine things in order to heal their cancer.
These nine key factors for Radical Remission are, in no particular order:
- Radically changing your diet
- Taking control of your health
- Following your intuition
- Using herbs and supplements
- Releasing suppressed emotions
- Increasing positive emotions
- Embracing social support
- Deepening your spiritual connection
- Having strong reasons for living
In Radical Remission, Dr. Turner states that these factors are in no particular ranking order — in her research, there was no “clear winner” among the factors. While some people focused more on one factor than the others, the majority of the survivors she interviewed did practice all nine of these key factors. These key factors are now considered “hypotheses” — that is, more research is needed to “prove” that these factors definitely improve the chances of healing from cancer or from other conditions.
Dr. Turner points out: “I don’t give medical advice nor do I even give advice, really. I’m just here to report on my research, and I can certainly say what radical remission survivors would do from a research standpoint.”
Using personal stories to illustrate each key factor, Dr. Turner shows how survivors overcame dire circumstances and diagnoses using modalities beyond the conventional treatments of surgery, chemotherapy, radiation and other “standard” cancer treatments. Interestingly, seven of these nine key factors that Radical Remission survivors reported using are psychosocial (mental/emotional) factors, while the other two are nutritionally-related.
At a time when psycho-oncology has come to the forefront of conventional oncology care, and when evidence-based integrative therapies are appearing in leading medical journals, Dr. Turner’s work could not come at a more opportune time. Dr. Turner’s unique and exemplary skill set: being a psychotherapist who then trained in social science research, and is a yoga teacher, has made her an ideal candidate for formulating, conducting and presenting this very timely research for the scientific community, as well as for creating an easily digestible format for the general public.
The Radical Remission Project website is an online community of patients, friends, family members, health professionals and Radical Remission survivors founded by Dr. Turner. The mission of the site is two-fold: to collect and verify as many radical remission cases as possible, and to connect Radical Remission survivors with current cancer patients to provide hope, inspiration and social connection. Everyone, whether sick or well, is encouraged to create a profile on the website.
Dr. Turner received her B.A. from Harvard University, and her Ph.D. from the University of California, Berkeley. She has recently adapted her Radical Remission work into a feature length screenplay entitled Open-Ended Ticket, and she can be found at https://kelly-turner.com/.
Dr. Turner also offers Radical Remission workshops, including an online course, “Radical Remission: Applying the 9 Healing Factors Into Your Own Life.” The course is for cancer patients and survivors, friends and family of cancer patients, or anyone who wants to prevent cancer. Additionally, Dr. Turner is working on a 9-part docuseries that will cover each of the 9 healing factors from her research, and will feature many of the Radical Remission survivors from the book.
The following is a conversation that I was honored to have with Dr. Turner in the summer of 2017.
Interview with Radical Remission author, Dr. Kelly Turner
Marianne Cirone: Dr. Turner, your book has been a New York Times Bestseller and a huge success. What insights have come to you since you have published this book?
Kelly Turner: Primarily, I realized that I wasn’t the only one interested in radical remission. The success of the book really shows me, more than anything, that people–just like I was–are fascinated by these real life cases. These are not made up cases. These people aren’t faking it. They really had cancer. And they really got better.
It’s fascinating, because the doctors can’t explain it. From a scientific standpoint, doctors simply have no hypothesis. We still can’t even fully explain it, but to hear how these people explain it in their own words is just a beautiful starting point to understand this phenomenon.
Marianne Cirone: How did your research start to recognize what has been happening for a long time, but has been under the radar of evidence-based medicine?
Kelly Turner: I think that before my research these cases were just sitting there, and no one was doing anything with them because they didn’t know what to do with them. That’s where I was sort of blessed to not be a medical doctor. I approached this as a psychotherapist. My master’s degree is in psychotherapy and counseling, and so I said, “Oh, so doctors don’t know why the people are getting well? So, let’s ask the person why they got well. Let’s go straight to the source and ask these people who were sent home on hospice to die, why they think it turned around.
Marianne Cirone: What type of model did you use for your research?
Kelly Turner: We need to look at these amazing survivors from every angle, including the medical angle, but in the absence of anyone doing that, from my perspective, without a medical degree–but with a PhD in social sciences research — I came at it and said, “Let’s apply anthropology to them.”
Anthropologists, when they go to the jungles of the Amazon and they encounter a new indigenous tribe of people that’s never had any contact with the outside world before, what do they do? Well, they apply anthropological research methods. They “go native.” They dress like the natives. They learn their language. They learn their customs. They gain their respect and trust, and then they just simply start observing and asking questions.
When you literally can’t explain anything at all and don’t even have any guesses about it, the only approach that really makes sense is the anthropological approach, which is to just gain their trust and ask them what they think is going on.
Marianne Cirone: That is amazing. I think that really speaks to the crossover of your different skillsets, that you could combine all these different parts of your background and look at it in a really unique way.
Kelly Turner: That’s where it feels like I was the right person for the job, because I didn’t have a medical degree and medical training, but I was a counselor who was used to asking questions and listening. I asked them, “Tell me everything you think might have contributed to your healing.”
I would schedule most of my interviews for an hour and they all went at least an hour and a half, if not two or three hours. That’s because no one had listened to these people before; no one had even asked them [how they healed].
I can’t tell you how many of the people I studied who told me that I was the first doctor or researcher — and, again, I always tell them a researcher, not a medical doctor — but they said, “You’re the first PhD or MD to ask me what I did to heal.” They said, “My oncologist didn’t ask me that.”
It’s upsetting for me to hear that over and over again, but it’s okay. That’s where things are and that’s what we have to deal with.
Marianne Cirone: It’s kind of a grass roots effort.
Kelly Turner: Exactly. My husband is a traditional Chinese medicine practitioner, and so I hear about chi from him. Then I’ve got the prana from my yoga training, and then we hear about the electromagnetic biofield from Western medicine and I’m like, “Oh, we’re all actually talking about the same thing.”
Marianne Cirone: I’m involved in the Society for Integrative Oncology, so I told my Committee for Patient Advocacy that we were going to do this interview and asked them what they wanted me to ask you, and a couple people asked specifically about the intuition that you mentioned in your book. And how do you overcome the resistance to when, as a patient, you start to step into your own power and then resistance comes from authority figures, family, whomever? What does science think about intuition and what do you do when the resistance comes up?
Kelly Turner: That was the one factor that was the most embarrassing for me to have to put in my dissertation. I was embarrassed because it’s not a scientific topic. I could spin all of the other factors into a term that was somewhat acceptable by Western medicine, right? Like “social support.” I specifically use that word – “social support” – because I didn’t want to call it “being open to receiving love,” which is how my research subjects described it.
If you use the word social support, that’s a term that researchers understand and they also understand how amazingly powerful social support is. In any cancer survival epidemiological study, if you take out social support, the [prediction] model falls apart. Social support is so powerful when it comes to [predicting] survival time.
Marianne Cirone: Right.
Kelly Turner: Things like “Having Strong Reasons for Living.” Well, what if you look at that as the opposite of depression? Depression meaning “no will to live.” So, a strong reason for living translates to a strong will to live, which means no depression.
Well, we have hundreds of studies on how depressed cancer patients die sooner. I felt like for all of the emotional factors, I could couch it in terms of reducing stress or increasing endorphins or increasing social support. For every single one of the seven emotional factors, I could reference some batch of studies that has been done, not only with health in general, but specifically with cancer patients. Scientists have done studies on stress and cancer, on depression and cancer, on social support and cancer.
Six out of seven of my mental/emotional factors were fully backed in science, and that felt really good because I thought, “Okay. I’m actually not saying anything new here. We actually already know this. We know this scientifically and we know this from a randomized, controlled trial.”
The one that I couldn’t say that for was intuition, because it simply hasn’t been studied. That made me really nervous, because I thought, “Okay. Every single person I interview is talking about this [intuition], but it hasn’t been proven in any studies.” This is what’s great about using anthropological methods, because is it’s not up to you what to write down. It’s up to them. That’s my job as a researcher when I’m using qualitative, anthropological methods: to step back and shut my mouth and write down what I observe.
It’s one thing when you’re studying Amazonian indigenous tribes and you say, “They do this crazy thing.” It’s a little harder when you’re studying cancer survivors and you say, “They do this ‘crazy’ thing, like following your intuition.” It was hard for me personally as a researcher to have to put that down in print, but I had to honor the findings. Then, I went on a hunt to try to make myself feel better about those findings and I hunted far and wide for any studies that have been done on intuition and let me tell you, not much had been done.
Marianne Cirone: Really? You do hear anecdotes about business people, like Conrad Hilton, who had this intuition about building a hotel or whatever.
Kelly Turner: You hear the anecdotes, but you don’t see scientific, psychosocial studies done. You actually find them done in business. A lot of the studies I found were about how consumers make decisions. I’ve found all these intuition studies about how consumers who followed their gut and just bought a car – bought the first car that really spoke to them – were found to be happier with their purchase three years later than the ones who exhaustively compared the top 20 models.
Marianne Cirone: That’s so interesting.
Kelly Turner: There’s a lot of intuition research done in the psychology of business, but that wasn’t helping me because I thought, “Okay, so intuition can help us feel better about the car we buy, but can it help our bodies heal from cancer?” That’s a big leap.
This is an area of study that needs to be explored, because there are important [intuition] studies that have been done but, unfortunately, I didn’t find any done with cancer patients. But there have been a few general health studies related to what you call intuition. I can call it “System Two” of the brain. You can call it your cerebellum – whatever you want to call it. The very back of your brain, right at the base of your brain, by the brain stem – that is the most ancient part of our brain. It’s also known as the reptilian brain. It is older and it predates the frontal cortex, which is when Homo sapiens really came up through the ranks and we stopped being chimps and started using tools.
That’s when the front of the brain, the frontal cortex, grew in size, and really sort of took over, but before that, when our brains were much smaller (and I’m talking about a really long time ago, when we were almost different types of humans), our frontal cortex was not as big and so a lot of what we were operating from was the very back of the brain, right above the spinal cord.
What we have found scientifically, and there are plenty of studies on this, is that the brain has two modes of operating. In neuropsychology, it’s usually referred to as ‘System One’ and ‘System Two.’ System One is the first one that existed. It’s the back of our brain, the reptilian brain.
I had to go to the neuro-psychology journals to figure out what’s going on when our instincts kick in. What’s going on in our brains when instincts kick in is that the back part of your brain takes over, and the front part shuts down.
Do you know how every cancer patient you’ve ever met says, “I don’t remember what happened when I was diagnosed. The last words I heard were, ‘You have cancer.’”?
Marianne Cirone: Yes, that’s true.
Right? You’ve heard that story from everyone. That’s because that’s actually what happens! They heard the words, “You have cancer.” Then they went into fear, which kicked on the instinctual part of their brain, the same part of the human brain that was alive and well when we were hunters and gatherers having to protect ourselves from bears and hurricanes all the time.
That [instinctual] part of the brain switched on — and because this is how our brains work–the second part of brain, the frontal cortex, which can calculate and analyze, makes to-do lists, etc. – shut down. Simply because you have a societal understanding of what the word “cancer” means in the Western world, which means something to be fearful of. As soon as you hear the words “You have this fearful thing,” you will most likely, unless you’re absolutely not afraid of cancer, have your brain switch into System One, and System Two will shut down. That means you are now operating by instinct.
Now, that doesn’t mean that the entire time you’re diagnosed and going to treatment you’re only in System One. It really kicks in in instances of fear and instances of intensity, such as that moment when you’re diagnosed. Or the moment you go into surgery, or the first CAT scan. The two days that you’re waiting for the test results.
People will say, “I wasn’t able to do anything for those two days. I couldn’t think straight.” Well, of course not, because your frontal cortex was shut down.
Once I found that body of literature and solid evidence about how our brains work, then my intuition finding made sense. I thought, “They’re saying intuition, but what scientists call it is System One.” Then, you get into the recent research from the past 15 years about the “second brain” in the gut. You have 100 million neurons in your gut – the exact, same brain cells that are in your brain are in your gut lining. Also, your gut brain cells, your gut neurons, can act independently of the brain. Your brain could be thinking of your to-do list and your gut can tell you, “Turn around quick. There’s a car coming.”
So, we have these two parts of our body that kick in: the base of the brain and also the neurons in your gut. Sometimes, if the base of your brain, System One, doesn’t kick in because your frontal cortex is too loud with your to-do list, then your second brain in your gut can independently kick in and give you a sudden awful feeling in your stomach. We have valid research that shows this. Once I found this research, I thought, “Phew! Alright. This is not woo-woo. This is evidence-based.”
The people who I interviewed were just using a word that researchers don’t like [“intuition”]. But, again, I’m trained in both qualitative and quantitative methods, and when you’re using qualitative methods, it’s most respectful to use the words that your subjects are using. So, that’s why I don’t call it “spontaneous remission,” because none of them call it that. They were actually really angry about it being labeled like that because they said, “This wasn’t spontaneous. I worked really hard to get here. It took me a year and a half to go from hospice to well.”
Marianne Cirone: Wow.
Kelly Turner: I used the word “intuition” because that’s what they used. Maybe, if I would have said, “Is the System One part of the brain operational?” I might have gained a few more medical fans, but I had to stay true to the subjects. Where the intuition comes into play is that it’s really this part of our brain taking over, and so number one, there is this body of research. Go back to SIO and tell them, “That’s where we need to look – in the neuro-psychology literature – to find this idea of System One/System Two and, also, the independent operation of your gut’s neurons. There are a couple of fascinating studies, not related to health, but related to how does this System One work in your body? What does it do? What can it do?
In my chapter on intuition, I quoted some of the studies, like the Iowa Card Study–which has been replicated so many times that we know it’s a fact–which is: your body knows danger long before your frontal cortex does. We know this because the subjects’ sweat glands opened up and their heart rate became more variable when they reached towards the card deck what was stacked against them. It took them approximately 10 cards before their sweat glands knew what was going on, but it took them 80 cards before their frontal cortex could actually describe what was happening.
Marianne Cirone: That’s amazing.
Kelly Turner: Right? After 10 cards, the body knew every time. As soon as they reached towards that dangerous deck, the sweat glands opened. The heart rate became variable. Their body knew safety, too. When they reached over to the safe deck, the sweat glands closed up and their heart rate became less variable, steadier.
The body knew after 10 cards. The frontal cortex knew after 80 cards; meaning, when the participants were asked to explain what’s going on here, after 80 cards they said, “Oh, I get it. This deck gives big wins followed by big losses, and this other deck gives slow and steady wins.” They were able to articulate what was actually going on after 80 cards. But their body knew under 10. That’s one of the coolest intuition studies I’ve read.
The Heart Math Institute is really taking the lead on questions like, “What is this instinct in our brain, what can it know, and when?” When you have that part of your brain that says, “Just call Jenny. Call Jenny. Call Jenny!” and you think, “Why am I going to call Jenny? I haven’t talked to her since we were in the third grade.” But your instinctual brain keeps repeating, “Call Jenny. Call Jenny.” So, you call Jenny and you are talking and then you end up saying, “Well, I got just diagnosed,” and she says, “Oh, my gosh, I just heard of this amazing doctor here in Reno.”
Maybe that’s why you were supposed to call Jenny, because she just told you the doctor who’s going to cure you. How does that work scientifically? Perhaps because the instinctual part of our brain knows the best path to safety well before our frontal cortex does.
There’s also this amazing study – it’s the Curtain Study done at Cornell that I mentioned in the book. It wasn’t a real curtain. It was a curtain on a computer screen, but the subjects had to choose which curtain the object was going to be behind. And the body knew the right answer every, single time, even when the subjects overrode that right answer with their logical mind and said, “I clicked on that one five times already. It can’t be that one again.”
Even when they hesitated and let their frontal cortex make the decision, their body still knew. As soon as they moved their mouse over the correct curtain, the sweat glands knew. Not only that, their bodies knew the right answer two to three seconds before the computer even randomly generated which curtain it was going to put it behind! It’s craziness that your body basically knows the future.
Marianne Cirone: And what do we do about dealing with the resistance to our intuitions? I wonder if women doubt their instincts more, too.
Kelly Turner: I think what makes us doubt them is the culture saying, “You’ve got to listen to the experts.” In my interviews, I always try to let the interviewer know that I’m not here to give advice. I’m not here to tell people to do these nine factors. This is not like an approach that I think we should all copycat and do. This is simply an approach that the radical remission survivors I’ve studied are using.
Marianne Cirone: Right.
Kelly Turner: I’m just relaying a phenomenon. I’m not necessarily advocating it. I have to say that because I want this research to continue and I think the minute I start to tell people prematurely, “Do these things. These things work.” That’s when I lose my credibility as a researcher.
What I can say is that you may want to do these nine factors because other people’s research has shown that they all boost the immune system, and boosting the immune system is always a good idea, whether you have cancer or not. If you’re a cancer patient who would like to boost your immune system, then sure. Work on these nine factors. That’s what I can say. When it comes to how I answer your question about what should be people do if they have resistance, it’s hard for me to give advice.
Marianne Cirone: I guess I’m asking from a standpoint that you have been a clinical therapist and the difficulty in making changes seems universal.
Kelly Turner: Yes. I can answer the question from the standpoint of my research, which is I can tell you how radical remission survivors handle this challenge. I’m happy to do it that way. Radical remission survivors that I’ve studied, some of them were blessed with really understanding friends and family who supported them every, single step of the way. Others were not. I would say more than 50% were not, so more than 50% of the people I studied had to deal with this resistance that you’re talking about. So, it’s a real thing.
Honestly, what a lot of them did is, if you want me to be brutally honest with you, is that a lot of them didn’t listen to their intuition at first. They took orders. They listened to the doctors. They did what their family members wanted them to do. They did anything and everything they were told to do, even though they had a little voice inside their head or a feeling in their gut that said, “No, no, no, no.”
So, many of them ignored that voice at first and for the people that I’ve studied, ignoring that voice was a mistake, in the sense that by ignoring it they did not get to full healing. The people that I’ve studied, again, I’ll just qualify this by saying, “the people that I’ve studied in-depth.” I can’t speak for anyone else, but for the people that I’ve studied, when they started listening to that voice, as opposed to ignoring it, that is when their healing started turning around and being more complete.
Maybe they got halfway with what they were doing – with what people were telling them to do, what the doctors were telling them to do – but it only got them halfway. Then, when they started listening to that intuition and doing these other factors as well, like tapping into why they want to be here, and saying no to things that drain them, and saying yes to things that give them joy– once they started doing these other nine factors, including listening to this voice as opposed to ignoring it, that’s when their healing started to turn around.
What do you do with that resistance? I mean, I think the lesson there that I take is that if you want to act like a radical remission survivor, you shouldn’t discount that voice from the beginning. You shouldn’t let six months or two years go by ignoring it. It should have a place at the decision-making table, at least that’s what the people I study say now. They say, “I wish that I would have just let it come to the table, let it have a voice.” Not necessarily always win or always be right, but at least have a vote in the matter.
That voice that might be saying, “Let me just try a really intensive diet change, combined with quitting the job I hate for two months, and let me see where that gets me. Let’s see if my numbers improve, or just even stay stable after two months of that, because my gut is saying that what I really need here is to leave the job that’s killing me, and to clean up my diet and start exercising and sleeping well again, because I haven’t done that in five years.”
Marianne Cirone: That’s great.
Kelly Turner: It’s great when that intuitive voice is telling you to do something that research shows is really healthy for you. Leave a job that’s stressful. Get your cortisol back on track. Get a good night’s sleep. Exercise every day. Return to your joy. Leave depression. Clean up your diet. All of those things right there have been shown in preventative studies to reduce the risk of cancer by almost 50%.
Marianne Cirone: That’s amazing that there is data to support all of that.
Kelly Turner: One of those factors, just on its own, reduces the risk of cancer by 50%, so imagine them combined. I definitely interview people who, as soon as they were diagnosed, they were drenched in fear, of course, because that System One took over. And then they heard this loud voice, because instinct takes over and they’re in fight-or-flight/survival mode. They were operating by instinct and that instinctual voice came and said, “Quit your job. Your job is killing you.” Then the frontal cortex said, “Oh, but I can’t quit. I can’t quit my job, because what about money, and what about this, and what about that?” So, they didn’t quit their job. And then they get cancer treatment and they have their health insurance, but then it’s not working and they’re getting closer to death as opposed to farther away from death. And then they quit their job, and then they’re suddenly so much happier.
It’s like the weight has been lifted from them. They realize they have 18 months of COBRA and someone from their church just donated to them, so they’re going to have great health insurance for 18 months and they say, “Okay. For the next 18 months, I’m just going to not worry about a job. I’m just going to focus on my health.” And then they spend the next 18 months exercising every day, reconnecting to what brings them joy, getting eight hours of sleep in complete darkness, totally cleaning up their diet, boosting their immune system, embracing their friendships again and allowing themselves to be supported and loved by them.
Well, lo and behold, 18 months later they’re better. Right when their COBRA runs out, they’re better. They get the clean scan. That’s not a made-up story. That was about somebody I just interviewed. These things really happen,
Marianne Cirone: Definitely.
Kelly Turner: This particular woman that I’m referencing, when we started talking about that voice that said, “You’ve got to leave your job. Your job is killing you,” she said to me, “I wish would have listened to it from the beginning, because it was right. It was right that what I needed to do to turn my immune system around was leave that job. That was one of the things I needed to do, and in fact, it was the first thing I needed to do,” and so she did it. She listened eventually. It just took her two years.
Marianne Cirone: I’m working with someone who is writing a memoir. I’m helping her edit it, and she had a terminal lymphoma diagnosis and then a breast cancer diagnosis, and she’s totally fine now, 15 years later.
Kelly Turner: Oh, my gosh.
Marianne Cirone: Her book is exactly like that. She even mentioned, in her book, that she read your book and she was like, “And I was happy to realize that I did all nine steps.”
Kelly Turner: That’s been really cool for me as a researcher to get all of these emails from new radical remission survivors that I haven’t met yet who say, “I was reading your book and it was like reading my diary. I did those nine things.” That’s great for me as a researcher, because that’s replicating the findings. That’s validating my findings. But please, please, please tell her to go to radicalremission.com and share her story!
Marianne Cirone: I will.
Kelly Turner: Because that’s where the research is continuing. I’m partnering up with this researcher from Tufts University. We’re applying for clinical trials. We’re taking cases from my website’s database and getting them verified and published. So, to help the medical field take these cases more seriously, we encourage anyone who has experienced a radical remission to share their story on our site.
What I really want is I want an exhaustive database that, ideally, has every, single radical remission case that ever happened in one place. That’s my goal, because once we have proof in numbers, then the scientific community won’t be able to ignore them anymore.
Marianne Cirone: That’s amazing. That’s a big goal, but I think you’re well on the way and there’s a lot of momentum.
Kelly Turner: Yes, people can submit their stories at www.radicalremission.com, so that our researchers can make note of it. They’re welcome to give as little or as much detail as they want, but even the demographics are helpful, such as how old were you when you were diagnosed, what was the type of cancer?, etc. In the checkboxes, we ask, “Did you do any of these nine factors? Yes or no?” Then, there is a part where, if they want to, they can share their whole healing story, but that’s optional.
Marianne Cirone: I’ve met so many people through the cancer center that were stage four diagnosis and they’re just doing great and they’re either in remission, or there is no sign of cancer, or they’re off all conventional medication.
Kelly Turner: Last December we upgraded our website and we now allow people to submit stories of healing even if they used chemo the whole way, which scientifically it’s harder to say then, “Well, what cured you? Was it the chemo or was it the other changes you made?”
But, in my opinion, if someone had stage four cancer and they’re well now, then we need to know about them. If they used chemo, plus these nine factors, and that’s what allowed them to endure the chemo and allow it to do its job, that’s something for oncologists to learn.
Which is to say, “How can we get stage four cancer patients on chemo to make it through to chemo? Oh, let’s have them do these nine things in addition [to the chemo].” So, really any survivor story at this point is helpful.
Marianne Cirone: And now you have written a screenplay also.
Kelly Turner: Yes. I’ve written a screenplay about radical remission and that’s actually my main focus right now, trying to get that film made. About 80% of my time right now is spent on that, which is really stressful, but also exciting.
Marianne Cirone: Is that funded now or are you still working on that?
Kelly Turner: That’s what we’re working on. We’re working on looking for investors. We have certain cast in mind, Hollywood “A” list cast, but you can’t really go to them until you have the money raised. We’re getting all of our pitch stuff ready and our budgets ready to go out to investors.
Marianne Cirone: That is so exciting.
Kelly Turner: Cross your fingers that we can get a major motion picture about radical remission out there in theaters.
Marianne Cirone: I think you have everything it takes to do it.
Kelly Turner: Let’s hope. For me it’s another way to tell the radical remission story. Some people read books about cancer. Other people won’t touch that, but they’ll go see a movie with their favorite actors in it, and if all they know is that it’s about healing, then maybe they’ll go see it, and then they’ll learn about this phenomenon of radical remission. It’s really just about trying to tell the radical remission story in a different way.
Marianne Cirone: Thank you so much for your time and for sharing your incredible research, Dr. Turner. We look forward to hearing more about your Radical Remission projects and will be looking forward to seeing your film in theaters.